When you purchase through our links, we may earn a commission at no extra cost to you. As an Amazon Associate, DreamSlumber earns from qualifying purchases. Learn more.
Conditions like osteoarthritis or rheumatoid arthritis can make you face common symptoms like nighttime joint pain, stiffness, and inflammation. Therefore, it becomes difficult to get the quality sleep necessary for your body’s recovery. However, you can manage flare-ups by following recommended sleep positions and a consistent bedtime routine with a supportive bedroom setup. You should also focus on daytime habits and know when to seek medical help.
Does the quiet of the night feel louder because of your aching joints? You are not alone. About 76.1% of arthritis patients suffer from insomnia due to nighttime inflammation. This cycle of “painsomnia,” where chronic pain causes fatigue and discomfort, can further deteriorate your arthritis symptoms. That is why it is important to figure out how to sleep with arthritis so that you can target the restorative deep sleep your body needs.
To manage your joint pain at night, you must find the best sleeping position for osteoarthritis and rheumatoid arthritis. The ideal position, when combined with a consistent bedtime routine and a supportive bedroom setup, helps you manage joint pain at night. Here, you will learn about actionable tips to manage flare-ups and identify when to consult a doctor. So, scroll down to discover our seven-step plan to break the cycle of arthritis pain at night.

Step 1: Understand How Arthritis and Sleep Affect Each Other
Before you learn about step by step guide to sleeping with arthritis, you must understand why your flare-ups become more intense at night. As your body follows a daily circadian rhythm, it naturally lowers cortisol (an anti-inflammatory hormone) while you sleep. However, pro-inflammatory proteins called cytokines spike in the early morning hours, leading to that familiar stiffness and heat. Let us understand this in detail:
The Pain–Sleep–Inflammation Loop
Chronic pain and sleep quality are related to each other. This is because arthritis pain keeps you from falling into a deep sleep at night. When your body does not get adequate rest, it increases its inflammatory response. This makes your brain more sensitive to signals of pain the next day, affecting your immunity and overall sleep cycle.
Different Arthritis Types, Different Nighttime Challenges
The sleep challenges you face at night also depend on the type of your arthritis:
- If you have osteoarthritis and sleep issues, your pain is of a mechanical nature. This means it comes from pressure on worn-down joints. This is when you need support to take off this weight from your joints.
- Those facing inflammation due to rheumatoid arthritis sleep problems suffer from heat, swelling, and whole-body fatigue. These symptoms show up due to an overactive immune system.

Step 2: Pick Joint-Friendly Sleep Positions and Adjust Your Pillows
To target deep sleep with arthritis, your sleeping position must keep your spine neutral and open your joints instead of compressing them. For this, you need a supportive bedroom setup and get accustomed to a basic position to minimize strain on your muscles. Here is how to sleep better with arthritis pain:
2.1 Choose the Best Basic Position for Your Body
Sleeping on your back is considered one of the best sleep positions for arthritis. It evenly distributes weight across the widest surface area of your body. Alternatively, side sleeping also helps support your hips in the correct alignment. However, you must avoid sleeping on your stomach as it may force your neck into a twisted position, hyperextending your back. This can intensify your morning stiffness.
2.2 Adjust Positions for Common Painful Areas
Try to adjust your sleep position to support your legs, spine, and lower back. To target painful areas, consider these tips:
If you are sleeping with hip arthritis or sleeping with knee arthritis knee pain, you must target neutral alignment by:
- Side Sleepers: Use a firm pillow and place it between your knees. Doing this will keep your top leg from pulling your hip downward and keep your pelvic area stable.
- Back Sleepers: Under your knees, place a supportive pillow. This will slightly bend your knees to open your hips and relieve pressure on your lower spine.
For sleeping with shoulder arthritis, your position must take off the weight from your joints.
- Avoid sleeping directly on your sore shoulder. Instead, sleep on your other side and hug a thick pillow against your chest to support your top arm.
- If you sleep on your back, place a folded towel or small pillow under your painful shoulder for support.
Your spine needs to be neutrally aligned to reduce any stiffness. For this:
- Keep your ears, shoulders, and hips aligned.
- If there is a gap between your waist and the mattress, tuck a rolled towel for extra lumbar support.
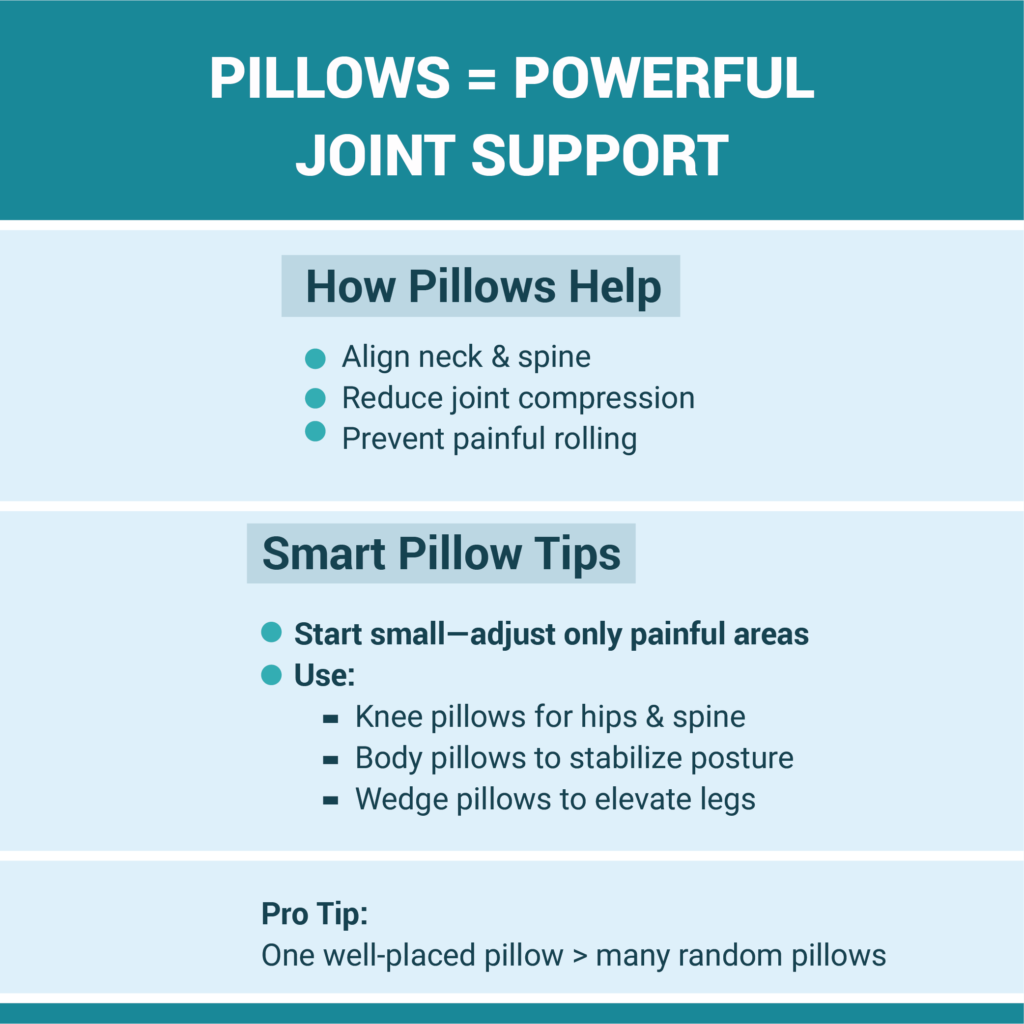
2.3 Use Pillows and Supports Wisely
It is common to use pillows for arthritis pain as they help you align your neck and shoulders, and can be used as knee and hip support. Follow these tips on how to use pillows to support joints at night:
- Start with small support adjustments according to where you feel the pain.
- Use body pillows to prevent rolling over and wedge pillows to lift your legs and reduce swelling.
- You can use a single pillow between the knees to get your body in a comfortable alignment that supports your spine’s curve.
Step 3: Create an Arthritis-Friendly Bedtime Routine
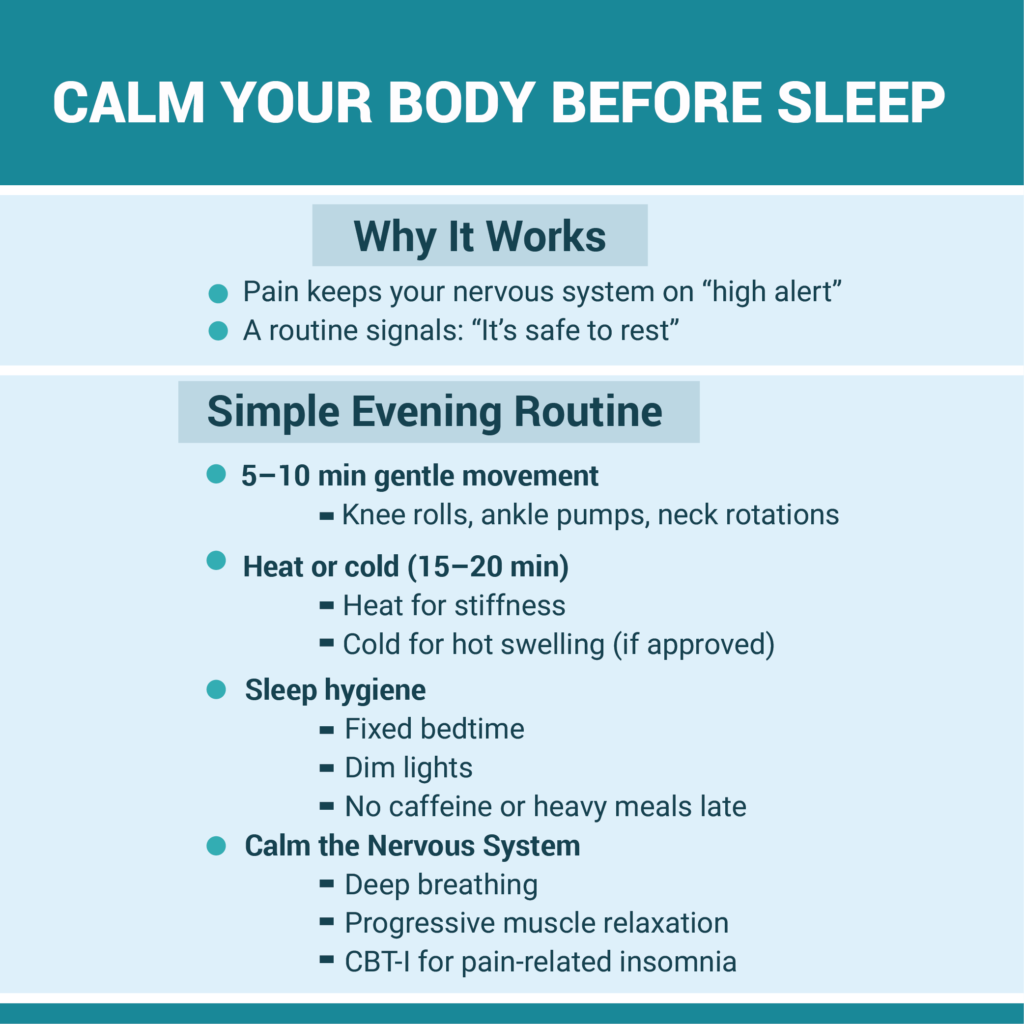
When you are in extreme pain at night, your nervous system interprets it as a signal of threat, keeping you up to stay alert. To manage this, a bedtime routine for people with arthritis helps calm down their bodies to signal that it is time to rest. Follow these tips to create an effective arthritis bedtime routine:
3.1 Loosen Up Gently Before Bed
Once you stop moving, your joint stiffness becomes more prominent. To gradually shift into sleep mode:
- Before bed, do 5 to 10 minutes of gentle stretches, like slowly moving your knees side-to-side.
- Get flat on your bed and perform ankle raises to improve the circulation of blood.
- Make sure these movements are gentle and pain-free, instead of treating them like intense workouts.
3.2 Use Heat or Cold Safely
Heat is a natural muscle relaxant. You can take a warm bath or use a heating pad for 15-20 minutes to soothe an arthritis flare at night. This also increases blood flow to stiff joints. Make sure you switch off the heating pad before sleeping to prevent the risk of burns. For acute and hot swelling, use a cold pack if your doctor recommends.
3.3 Practice Good Sleep Hygiene
You must also follow basic arthritis and sleep hygiene rules to improve your sleep quality. Create a sleep schedule for each night and dim the lights to wind down 30-60 minutes before bed. Try to avoid heavy meals or caffeine in the evening. Create a calm environment to slow down your racing mind and fall asleep.
3.4 Calm Your Nervous System
To calm your nervous system, use techniques like progressive muscle relaxation or slow and deep breathing. If your mind races due to anxiety, opt for Cognitive Behavioral Therapy for Insomnia (CBT-I) and arthritis programs. These therapies offer evidence-based solutions to treat joint pain and insomnia by changing your perception of sleep.
An Arthritis-Friendly Evening Routine Checklist:
- 1 Hour Before Bed: Turn off bright screens and dim the lights in your room. This helps your brain produce melatonin.
- 45 Minutes Before Bed: Take a warm bath or apply a heating pad to stiff and achy joints for 15-20 minutes.
- 30 Minutes Before Bed: Perform 5-10 minutes of pain-free movements, such as slow neck rotations or ankle pumps.
- 15 Minutes Before Bed: Try slow and diaphragmatic breathing or a brief body-scan meditation.
- At Bedtime: Make sure pain relievers, water, or topical creams are within easy reach to avoid middle-of-the-night disruptions.
Step 4: Optimize Your Bed, Bedding, and Bedroom Environment
Even if you follow a routine and sleep in the best position, if your bed setup is not supportive, these efforts may go in vain. That is why you need a pressure-relieving setup with engineered space that reduces mechanical stress on your joints. Follow these tips on how to set up your bed for arthritis-friendly sleep and find which mattress is best for arthritis and back pain:
4.1 Choose Supportive, Pressure-Relieving Surfaces
A medium-firm mattress is often the most recommended investment for people with arthritis. Clinical research suggests that soft mattresses must be avoided as they may sink your body too deeply. It pushes your body to get stuck in one position, twisting your spine. Instead, choose a medium-firm surface. It supports your skeleton while cushioning pressure points like hips and shoulders. If you do not want to replace your current mattress, you can invest in an arthritis-friendly mattress topper.
You can choose from:
- Hybrid mattresses: These use foam to contour the body and springs to give a responsive surface to ease movement.
- Memory foam: These work best for pressure relief. However, their surface can be too plush for heavier sleepers and restrict their movement.
- Innerspring: These mattresses are firm and easier to move on. However, they lack cushioning to support the sensitive joints at night.
4.2 Dial in Your Pillows and Supports
To adjust your position and set up, use a head pillow to keep your neck neutral with your shoulders and spine. You can also invest in an adjustable bed frame that lifts your torso and lower body slightly to keep you in a zero gravity position. This relieves your pressure points, improves blood circulation, and reduces nighttime pain. Alternatively, you can place a wedge pillow to achieve this setup on a budget.
4.3 Get the Room Temperature, Light, And Noise Right
At night, keep your bedroom cool and dark (around 65°F/18°C) to reduce inflammation. Use breathable bedding like cotton or bamboo to stay warm without overheating. To reduce street noise, install a white noise machine to distract your brain from pain signals.
4.4 Make Getting In and Out of Bed Easier
With arthritis, you may face mobility issues, and hence, it is important to adjust the height of your bed. When sitting on the edges, your feet must touch the floor with your knees bent at right angles. This can be achieved with about 20-23 inches. If your bed is too low, you can use bed risers. If the bed is too high, use a step stool with a handle. Consult an occupational therapist to give you correct advice on transfer techniques if you face mobility issues.
| Feature | Why it helps | Things to watch |
| Medium-Firm Mattress | Balances support and cushion; easier to move on. | Too firm can hurt pressure points |
| Heavy Blankets | Can provide comforting sensory input | Too heavy can trap feet or pressure-sensitive toes. |
| Satin Sheets/Pyjamas | Reduces friction, making it easier to slide/turn over. | It can be slippery, so be cautious when sitting on the edge. |

Step 5: Adjust Daytime Habits that Make Night-Time Sleep Easier
In addition to following healthy habits at night, you must also focus on improving your daytime routine. You must engage in daily movement, watch your caffeine intake, and reduce stress levels. Here are the tips on pacing yourself during the day to lower flare-ups at night:
5.1 Move Regularly, But Don’t Overdo it
For arthritic joints, regular motion is very important to manage the stiffness. For this, include low-impact exercises like walking, swimming, or tai chi in your daily routine. These keep your joints lubricated, and your body gets tired at night to slip into rest mode. Please note, you must not overdo these exercises to avoid crashing the next day due to pain.
5.2 Manage Fatigue and Nap Smart
Arthritis fatigue and sleep are interconnected. You need deep rest at night to manage your joint pain, so avoid taking late-afternoon naps. Daytime snooze can reduce your sleep drive, keeping you up all night. Instead, you can take a shorter power nap before 2 p.m. or just rest without falling asleep.
5.3 Watch What and When You Eat and Drink
Avoid taking heavy meals an hour before bed, as it may cause indigestion, leading to fragmented sleep at night. Limit the caffeine and alcohol intake when it is close to bedtime. To get personalized advice, consult your clinician to get a medication schedule and diet chart.
5.4 Support Your Mood and Stress Levels
Living with chronic pain means you are constantly under stress and anxiety of dealing with inflammation each day. You can opt for counseling, join support groups, or take the help of relaxation apps to ease your mind. Talking about your mood changes to your doctor can help you get targeted solutions.
Daytime Habit Checklist:
- Did I move my body today?
- Did I stop caffeine after 2 p.m.?
- Did I pace my activities to avoid any pain the next day?
- Did I spend some time outside in natural light?

Step 6: Have a Simple Plan for Nights When Pain Wakes You Up
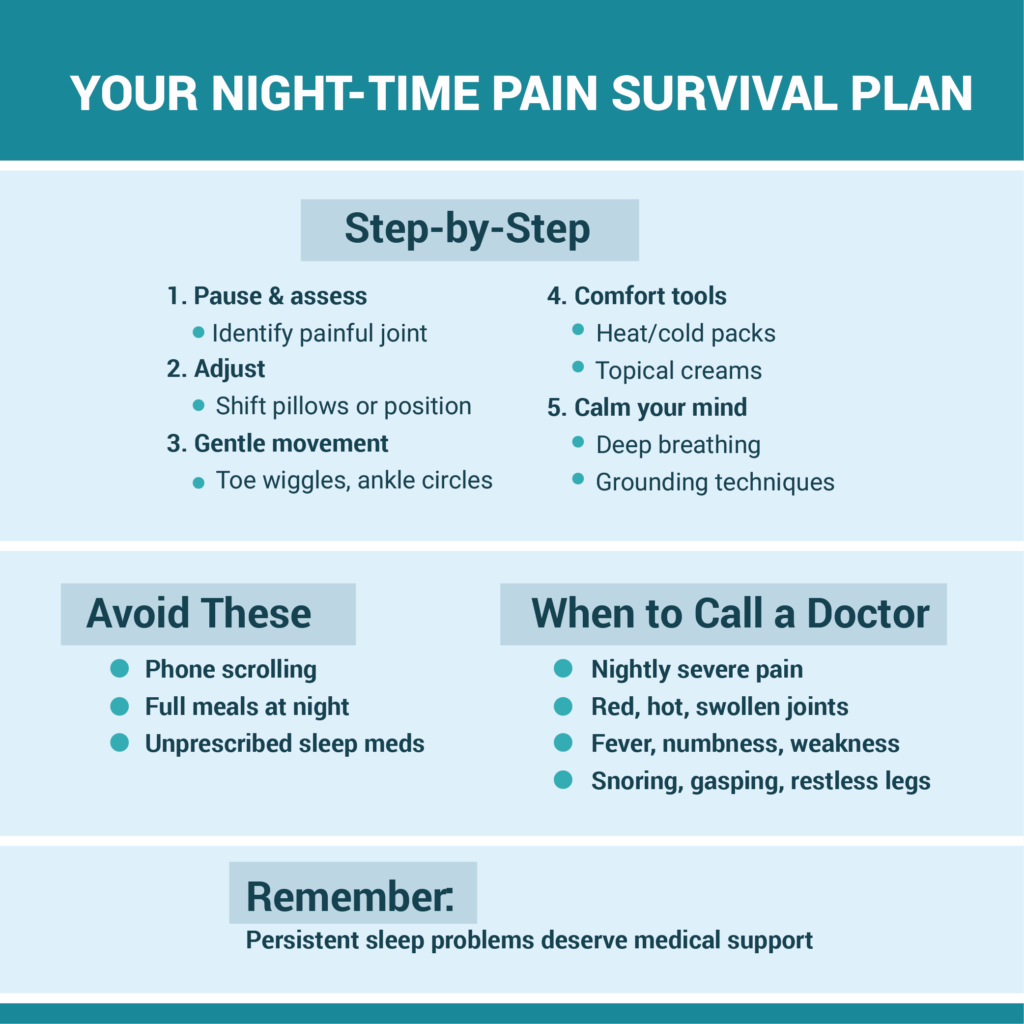
If you are diagnosed with arthritis, it is best to stay prepared for the painful nights. Instead of searching for ‘night-time arthritis pain what to do’ solutions online and panicking, you can follow these simple steps:
6.1 Pause and Adjust Your Position
In case of shooting pain, pause your racing mind and assess the area of pain. After that, grab a pillow or shift the existing one to support your joints. Gradually, roll over to your non-painful side and straighten your bent knee.
6.2 Add Brief, Gentle Movement
In case of stiffness, avoid lying still and instead, engage your joints in slow movements. You can wiggle your toes, do ankle circles, or bend and straighten your knees. If you do not get any relief, gently get out of bed and walk slowly to lubricate your open your joints.
6.3 Use Approved Comfort Tools
Create a comfort kit and place it on your nightstand. Include a heat pack, a cold pack (if approved by the doctor), and topical creams that provide a cooling or warming sensation.
6.4 Calm Your Thoughts So You Can Fall Back Asleep
After you get comfortable in bed, calm your anxiety by following any relaxation technique. You can focus on your senses of feeling, hearing, etc., to ground yourself. Use breathing exercises to let your nervous system relax.
6.5 Avoid Sabotaging Your Next Night
When in pain, your first instinct may be to pick up your phone and search for solutions, but the blue light may further wake you up. Also, refrain from eating a full meal at night or taking sleep medication that is not prescribed.
Mini-Protocol: If You Wake in Pain
- Assess: Do I need to move or support a joint?
- Adjust: Shift pillows or position.
- Soothe: Use heat/cold or topical cream if needed.
- Breathe: Do 10 deep breaths.
- Reset: If not asleep in 20 mins, go to a dim room and listen to quiet music.
Step 7: Know When To Talk To Your Doctor or a Sleep Specialist
If you are following all these steps and see no improvements, it is best to consult a medical professional. Your rheumatologist and therapist can offer treatments that will target the root cause of pain more effectively. Let us discuss when to see a doctor about arthritis and poor sleep:
7.1 Red Flags You Shouldn’t Ignore
Look for these signs in your body:
- Persistent, sudden, and shooting pain each night.
- New swelling, redness, or heat in a joint.
- Fevers, night sweats, or sudden weight loss.
- New weakness, numbness, or tingling in your limbs.
7.2 Sleep Disorders That Appear With Arthritis
- Arthritis and Sleep Apnea: If you suffer from rheumatoid arthritis, check if you snore at night, gasp for air, or wake up with dry mouth or headache frequently.
- Restless Legs Syndrome (RLS) and Arthritis: If you notice an urge to shake your legs at night, this may signal RLS. It is treatable and needs targeted diagnosis.
- Insomnia: You may suffer from anxiety-induced insomnia if you face difficulty falling asleep for several nights.
7.3 How Your Health Team Can Help
You can consult a sleep expert to rule out the symptoms of sleep apnea, insomnia, or RLS. To learn gentle arthritis-friendly movements, you can seek help from a physical therapist. A psychologist can guide you through CBT-I techniques to treat underlying issues.
7.4 Bring Useful Information To Your Appointment
To help your doctor understand your condition better and offer personalized advice, maintain a daily log of sleep and pain. Bring this to your appointment and mention:
- What time did you go to bed and wake up?
- How many times have you woken up in pain?
- Your pain level (0-10) in the morning.
- What you did during the day (exercise, caffeine, stress).
The table below summarizes the common symptoms and the help you can seek:
| Symptom | Who to Contact | Urgency |
| Loud snoring/gasping | Primary Care/Sleep Specialist | Routine appt (weeks) |
| Hot, red, swollen joint + fever | Rheumatologist/Urgent Care | Immediate/Same Day |
| “Creepy-crawly” legs at night | Primary Care | Routine appt |
| Consistently waking in pain | Rheumatologist/PT | Routine appt |

Frequently Asked Questions
How many hours of sleep should I aim for if I have arthritis?
For arthritis, you should get at least 7 to 9 hours of sleep each night, standard for all adults. This will help you manage your painful symptoms better and let your body repair muscle tissues. It is important to focus on the quality of restorative sleep instead of the hours spent.
What is the best sleeping position for arthritis in the knees and hips?
Back sleeping with a pillow under your knees is the best sleeping position for arthritis in knees and hips. Other than this, side sleeping is also recommended for some of the arthritis patients. Both positions keep the hips and spine neutral and relieve pressure points.
Can a better mattress or pillow really help with arthritis pain at night?
Yes, a medium-firm arthritis-friendly mattress and a contouring/supportive pillow can support your joints, reducing pain at night. The mattress contours your body to cradle the sensitive zone and provide pressure relief benefits. By placing pillows strategically, you can offload pressure from your shoulders, hips, and knees.
Is it safe to use a heating pad or electric blanket all night with arthritis?
While a heating pad or an electric mattress helps soothe the painful zones in your body, keeping them on for too long is not recommended. It may cause severe burns, worsening your nerve damage, or poor circulation symptoms. It is suggested to use these for 15 to 20 minutes short sessions to relax muscles and turn off before you sleep.
Why does my arthritis feel worse at night, even if I take my medication?
At night, your body’s circadian rhythm makes the levels of cortisol drop. At the same time, inflammatory substances called cytokines increase. This biological process leads to a temporary arthritis flare at night, even if your medication is managing pain during the day.
When should I ask my doctor about a sleep study or seeing a sleep specialist?
Consult your doctor or sleep specialist if your insomnia becomes more frequent despite following arthritis-friendly practices. See if your partner notices your loud snoring, breathing issues, or gasping for air during sleep. These may be due to sleep disorders that often accompany arthritis and require professional diagnosis.
Can better sleep reduce inflammation from arthritis over time?
Yes, when your body gets consistent restorative rest, it effectively repairs damaged tissues and releases proteins to reduce inflammation. This further helps manage your nighttime anxiety, helping you reduce joint pain and inflammation in the long term. It also helps your medications work for your body, reducing daytime discomfort.
Conclusion
When looking for effective solutions on how to sleep with arthritis, it is important to understand that it is a gradual process that requires patience. To manage your symptoms, you must get used to the joint-friendly back sleeping position and create a realistic arthritis-focused bedtime routine. For this, set up your sleep sanctuary by using a medium-firm mattress and supportive pillows. Follow consistent and gentle daytime habits, and keep a comfort kit handy to stay prepared on painful nights. Lastly, seek regular consultation from your rheumatologist and sleep specialist to get personalized advice.
This is not an overnight solution, so start slow by picking one or two strategies from this guide. Follow a few doable steps and track if you see any improvements. Be patient with yourself, and discuss your progress with your doctor.


