When you purchase through our links, we may earn a commission at no extra cost to you. As an Amazon Associate, DreamSlumber earns from qualifying purchases. Learn more.
If you want to sleep better with fibromyalgia, you first should optimize your pillow setup to support sensitive pressure points. Further, make sure you have consistent temperature regulation in your bedroom. Follow a strict bedtime and wake-up schedule and address common disruptors like sleep apnea, restless legs syndrome, or insomnia. If you do not notice improvements in painful flares despite these adjustments, seek guidance from a clinician to manage your symptoms more effectively.
Nights with fibromyalgia may feel endless when you are physically exhausted, yet your body is unable to settle into rest. When searching for solutions on how to sleep with fibromyalgia, you must recognize that your struggle comes from central sensitization that results in insufficient rest. Moreover, chronic pain, fatigue, and insomnia create a biological cycle that is difficult to break without a plan.
Sometimes hidden disruptors like restless legs syndrome (RLS) or sleep apnea make deep sleep even more elusive. This guide offers a 2-to 4-week strategy to help you reclaim your nights by refining your sleep routine and daytime pacing. You will learn about the use of a heating pad, a weighted blanket, and strategies like CBT-I to help you target restorative rest. So, keep reading to get a step-by-step plan along with troubleshooting for flare nights and advice on exactly when to seek professional help.
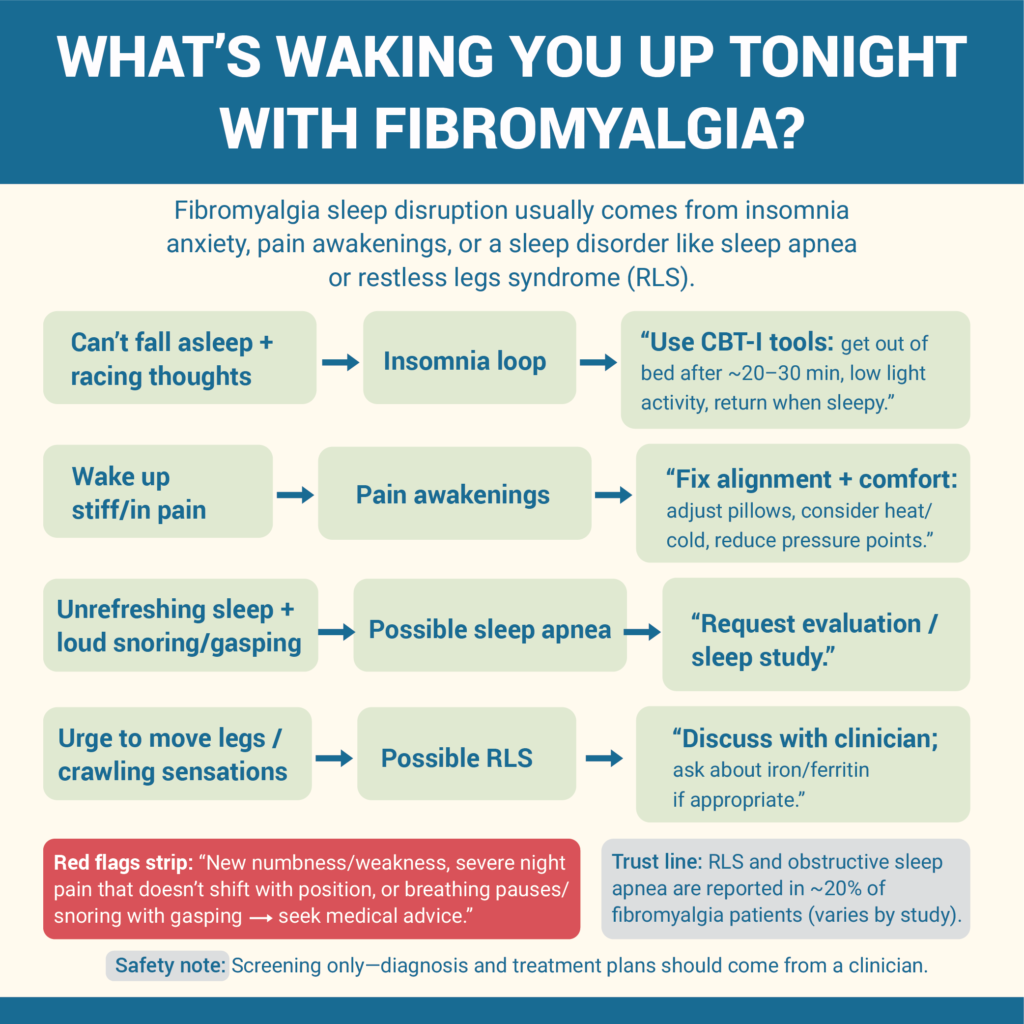
Step 1: Identify What’s Keeping You Awake With Fibromyalgia (Pain, Insomnia, or a Sleep Disorder)
If you find yourself staring at the ceiling for hours, you may be stuck in a fibromyalgia insomnia cycle. On the other hand, if you wake up repeatedly due to stiffness, it may be due to pain flare-ups. For many, this vicious cycle involves pain-causing nonrestorative rest, which in turn makes you more sensitive to pain the next day. Here’s what you need to check:
- Can’t Fall Asleep: This points to an insomnia loop in which you feel anxious when you are unable to sleep. It keeps the brain too active for rest.
- Wake Up from Pain: This may occur if your sleep environment is unsupportive and does not provide temperature regulation to keep your nerves calm.
- Unrefreshing Sleep and Snoring: If you wake up feeling like you have not slept at all and often find yourself gasping for air, you may need an evaluation for sleep apnea. This is a common condition that occurs in nearly 20% of fibromyalgia sufferers.
- Urge to Move Legs: If you experience a crawling sensation or an urge to move your legs, this may be due to restless leg syndrome.
Red Flags for Medical Evaluation
You can manage all the minor fibromyalgia-related sleep issues at home. However, it is important to look for certain symptoms that may be serious. Seek medical advice if you experience:
- New neurological symptoms like numbness.
- Severe night pain that does not change with position
- Noticeable pauses in your breathing during sleep.
Decision Tool: Which problem is yours tonight?
Use this flowchart to route your symptoms to the right relief strategy:
- Racing thoughts, but low physical pain? → The Insomnia Loop. Focus on CBT-I and calming your sleep anxiety.
- Comfortable but wake up in a “flare”? → Pain Awakenings. Adjust the firmness of the mattress or use a heating pad.
- Waking up gasping or with “fidgety” legs? → RLS/Apnea. Consult a specialist for a sleep study to rule out sleep-disordered breathing or periodic limb movements.
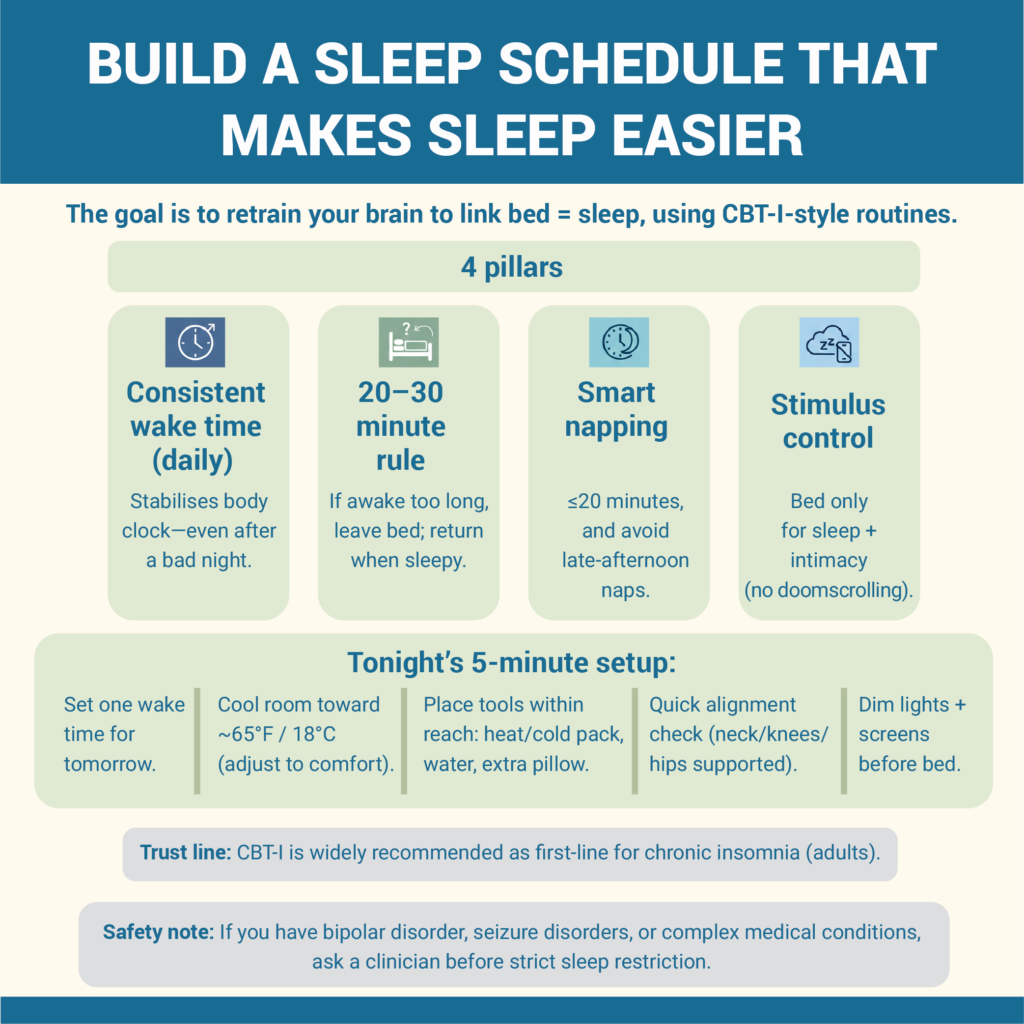
Step 2: Set a Fibromyalgia-Friendly Sleep Schedule That Lowers “Insomnia Pressure”
If you want to lower your insomnia pressure, train your brain such that it associates the bed with sleep. Many experts recommend CBT-I (Cognitive Behavioral Therapy for Insomnia) as a primary treatment. This is because it addresses the behavioral habits that often worsen fibromyalgia. While these changes take time, research shows that improving sleep quality can reduce the overall perception of pain. Here’s what you should do:
- Follow a Consistent Wake-Up Time: Wake up at the same time every day, even on the days when you had poor sleep. This makes your circadian rhythm stable.
- The 20-minute Rule: If you are awake for more than 20-30 minutes, get out of bed and do a low-light activity like reading until you feel sleepy.
- Smart Napping: Avoid taking long naps that exceed 20 minutes during the day. Make sure you do not nap after 3:00 PM to ensure you can fall asleep by bedtime.
- Stimulus Control: Use your bed only for sleeping and intimacy to establish a mental link between your mattress and resting.
Tonight’s 5-minute setup
- Set the Alarm: To wake up consistently at the same time, set an alarm such that you get at least 7-8 hours of sleep. Avoid creating an early alarm to target REM sleep.
- Cool the Room: Set your temperature to around 65°F (18°C) to prevent waking up due to overheating at night.
- Keep Pain-Relieving Tools Handy: On your nightstand, keep a heat pad, weighted blanket, and other tools within reach.
- Dim the Lights: Switch off bright lights in your bedroom and device screens an hour before bed.
- Check Your Alignment: Use extra pillows if you want to sleep on your side or back to support your pressure zones.
If you find it difficult to sleep at night due to stress, create a mindful wind-down routine. This will help you calm your racing mind before starting sleep restriction therapy.
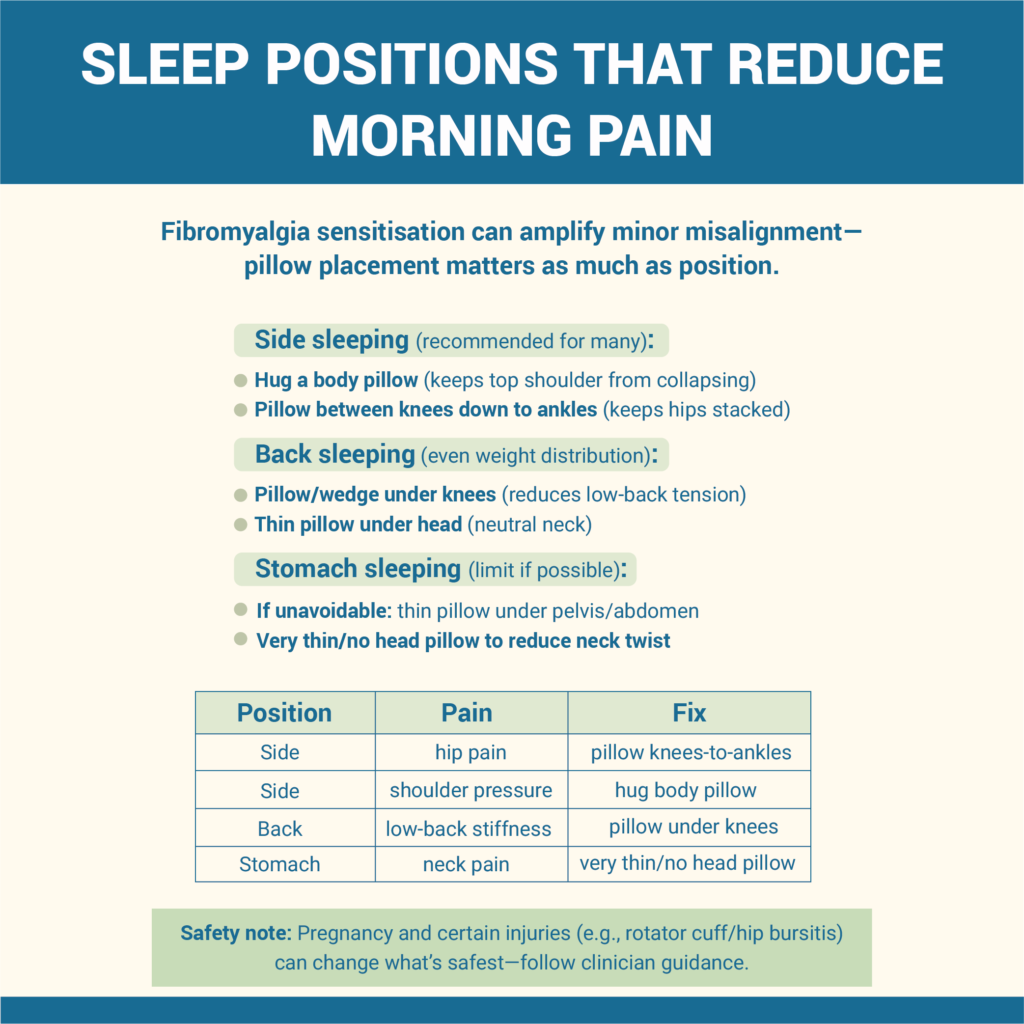
Step 3: Choose the Best Sleeping Positions For Fibromyalgia (Reduce Pressure Points and Morning Pain)
The best sleeping position for fibromyalgia sufferers is one that reduces the pressure on sensitive pressure zones and maintains spinal alignment. Fibromyalgia includes central sensitization, which means your body may see even slight misalignments as intense pain. This makes pillow support a non-negotiable tool for relief.
You can experiment with these clinician-aligned setups to manage the morning stiffness:
Side Sleeping
Recommended by many experts, this is the most comfortable position that reduces muscle tension. To use a pillow setup for fibromyalgia side sleeping shoulder pain, hug a body pillow to keep your top arm elevated. Next, place a firm pillow between your knees (extending down to your ankles) to keep your hips level. Use an engineered mattress for side sleeping to make sure you get the right support.
Back Sleeping
If you suffer from shoulder pain and fibromyalgia issues, sleep on your back to distribute your weight evenly on the surface. To enhance comfort, use a wedge pillow under your knees to reduce pressure on the lower back. Keep a thin pillow under the head so that your neck is supported and is not forced too far forward.
Stomach Sleeping
This position must be avoided as it may cause excessive neck strain. However, if you have to sleep face down, use a thin pillow under your pelvis or abdomen. This setup will keep your lower back from arching. It also protects your spinal curve even when you are forced into this position
Position and Pain Adjustment Table
| Position | Pain Pattern | Adjustment |
| Side | Hip pain or “bursitis.” | Place a pillow between your knees down to the ankles to keep your hips stacked. |
| Side | Shoulder pressure | Hug a body pillow to prevent the top shoulder from collapsing forward. |
| Back | Low-back stiffness | Slide a medium-firm pillow under your knees to flatten the lumbar spine. |
| Stomach | Neck pain/stiffness | Use a very thin pillow or no pillow at all for the head to keep the neck neutral. |
Note: If you have specific concerns like a rotator cuff injury or hip bursitis, avoid certain positions like stomach sleeping entirely. If you are pregnant, side sleeping with an extra pillow support is the safest and most comfortable option.

Step 4: Build a “Sensory-Safe” Sleep Environment For Fibromyalgia (Temperature, Fabric, Light, Sound)
For some, fibromyalgia is accompanied by allodynia, where even the weight of a heavy blanket or a thick sheet may feel painful. To prevent this, you must create a sensory-safe sleep environment. It requires a bedroom setup that regulates temperature and light to prevent sensory overload that disrupts your bedtime. Follow these tips:
Temperature Strategy
Your bedroom temperature and fibromyalgia night sweats are directly related. For best comfort, keep the baseline temperature of around 65°F (18°C) so that your core body temperature is low. You can also use a heating pad or hot water bottle to calm the sore muscles while keeping the surrounding air cool.
Fabric Strategy
Opt for a soft and low-friction fabric, such as bamboo or silk. These are lightweight and organic, and do not irritate your sensitive skin. Make sure your night pajamas do not have a tag and have flat seams. This will prevent any physical irritation that may wake you up from deep sleep.
Light/Sound Controls
Sleep in a dark room and use blackout curtains to avoid any light leaks. Alternatively, you can also keep an eye mask handy to block any light in the room. To keep the sleep environment calm, use a white noise machine. These tools prevent unnecessary light and sound that may startle your nervous system and impact melatonin production.
Bedroom Audit in 10 Minutes
- Is the room cool (65°F), and do you have a heating pad ready?
- Are your sheets soft, and is a thick blanket or a cooling layer nearby?
- Do you have enough pillows for knee, back, and arm support?
- Are the blackout curtains closed and white noise on?
- Is your phone out of reach and the blue light filter on?
If you constantly suffer from overheating at night, swap your regular bedding for moisture-wicking one. Moreover, if fibromyalgia is your main barrier, choose a specialized mattress to ensure your base is providing the right support.
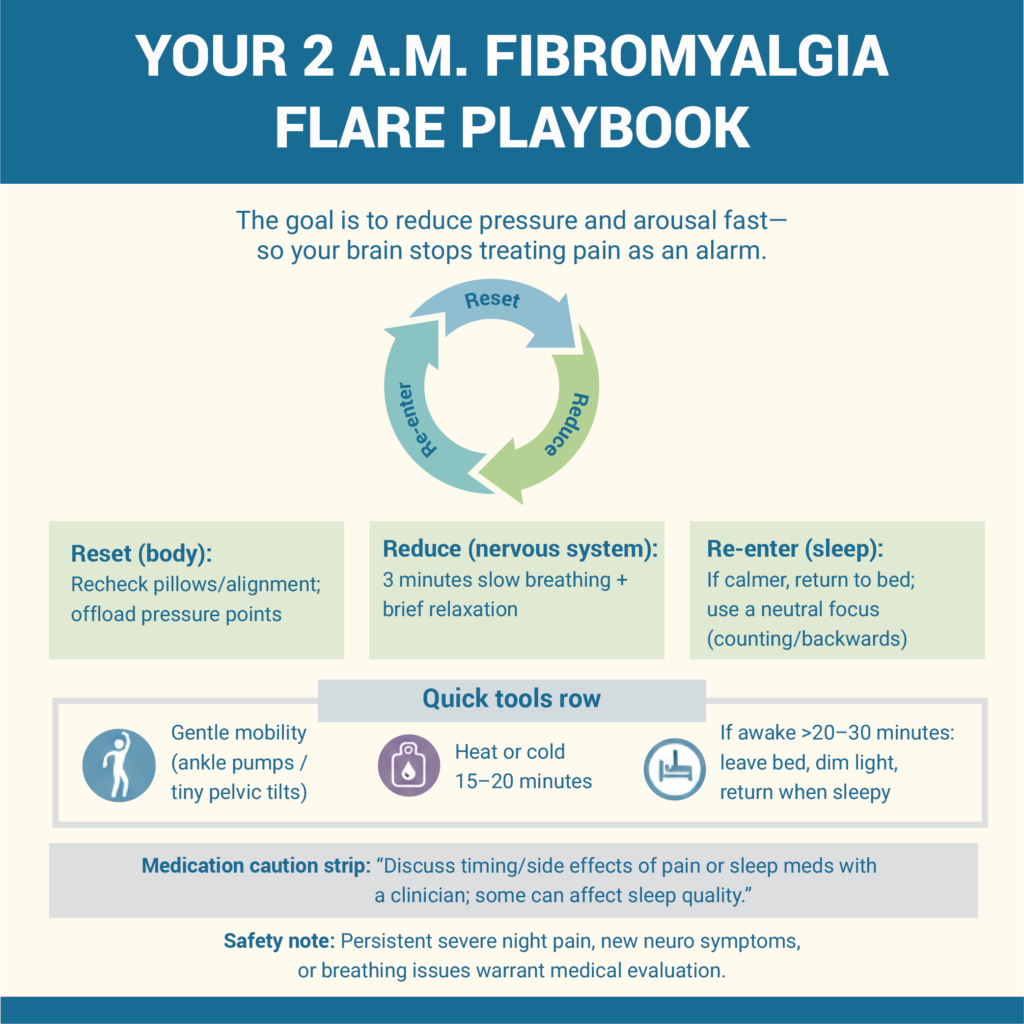
Step 5: Create a Nighttime Pain Plan That Helps You Fall Back Asleep During Flares
Your fibromyalgia pain flare-ups may keep you up at 2 a.m., causing you anxiety that further impairs your recovery. To manage this, your primary goal is to lower your body’s alarm system that keeps you alert. In this condition, your brain may interpret even minor discomfort as a major flare, resulting in insomnia. That is why you need a pre-set protocol that reduces your overall stress of what to do when fibromyalgia pain wakes you up.
When you wake up due to pain, follow these steps to reset your system:
- Reset Your Position: First, check your pillow support and alignment to make sure your bodyweight is not putting extra stress on your pressure points.
- Slow Your Breathing: Before bed, engage in 3-5 minutes of deep and diaphragmatic breathing. This tells your nervous system that it is safe to relax and lose control.
- Use Gentle Movement: If you feel stiff, do low-intensity mobility exercises like ankle pumps or small pelvic tilts.
- Apply Heat or Cold: Use a heating pad or a cold gel pack, whichever provides you the most relief, for about 15-20 minutes on painful areas.
- Leave the Bed If Needed: If you are still awake after 20 minutes, get out of bed to sit in a dimly lit room. Continue this until you feel sleepy again to avoid a negative mental link with your mattress.
The ‘Reset-Reduce-Re-enter’ Model
You can utilize these fibromyalgia sleep tips that actually work:
- Reduce Pressure: Check your positional alignment and enhance your comfort using pillows to remove pressure from the joints and sensitive zones.
- Reduce Arousal: Use CBT-I techniques like progressive muscle relaxation to lower the mental stress of the pain.
- Re-enter Sleep: If your body feels slightly relaxed, go back to bed and focus on a neutral mental task, like counting backwards. This helps you re-enter a sleep state.
Note: Use a barrier (like a cloth cover) when applying heat or cold therapy to avoid skin irritation, and avoid sleeping directly on top of it. You must discuss the timing of your pain medications with a clinician. This is important because some sedatives can interfere with your overall sleep architecture.
Your 2 a.m. Checklist
- Fix your pillows to offload pressure points.
- Three minutes of box breathing and five ankle pumps.
- Use a heating pad (with an auto-shutoff) to soothe muscles.
- If still awake, control stimulus by leaving the bedroom.
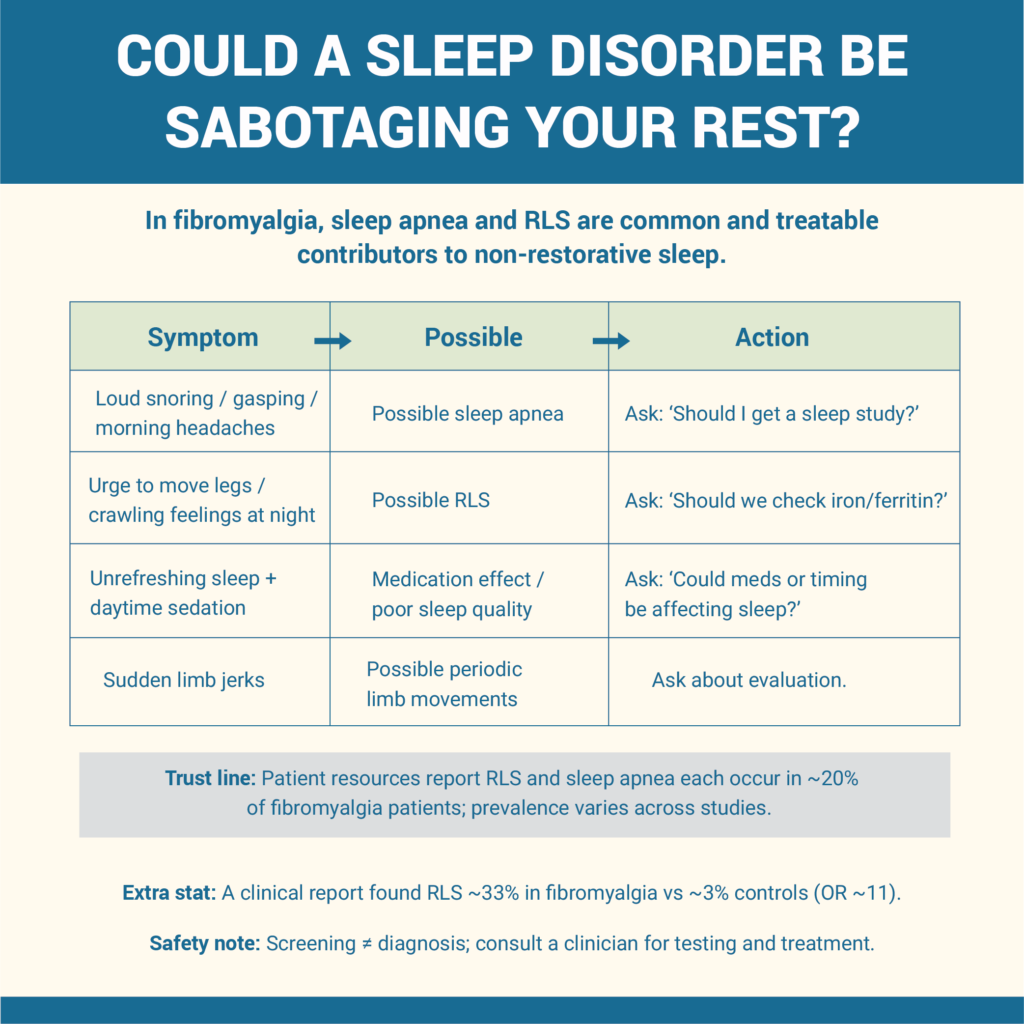
Step 6: Check for Sleep Apnea, Restless Legs, and Other Common Sleep Disruptors in Fibromyalgia
If your poor sleep quality symptoms have lasted for weeks, it is time to do some self-assessments. Most fibromyalgia sufferers do not get restorative rest due to underlying health issues such as sleep apnea, RLS, and chronic inflammation. ScienceDaily research shows that RLS is common among fibro patients. It is 11 times more likely to occur than other issues, affecting 33% of those suffering from it.
To identify these comorbidities:
- Sleep Apnea: Look for the signs of loud snoring at night, gasping while breathing in sleep, or if you wake up with morning headaches.
- Restless Legs: At night, if you experience an urge to move your legs, it may be due to RLS. Consult your doctor and get your ferritin (iron) levels checked, as low iron may trigger it.
- Medication Effects: If you take pain relief or anxiety medicines, they may cause insomnia or drowsiness during the day.
| Symptom | Possible Cause | What to Ask Your Clinician |
| Gasping or heavy snoring | Sleep apnea | “Should I get a sleep study for fibromyalgia sleep problems?” |
| Fidgety leg sensations | Restless legs syndrome | “Should I get my iron and ferritin levels checked?” |
| Waking up feeling unrefreshed | Poor sleep | “Are my current medications affecting my sleep?” |
| Sudden limb jerks while asleep | Periodic Limb Movement Disorder | “Could my leg movements be disrupting my sleep?” |
Disclaimer: These screening signs are for reference only and do not replace a professional diagnosis.
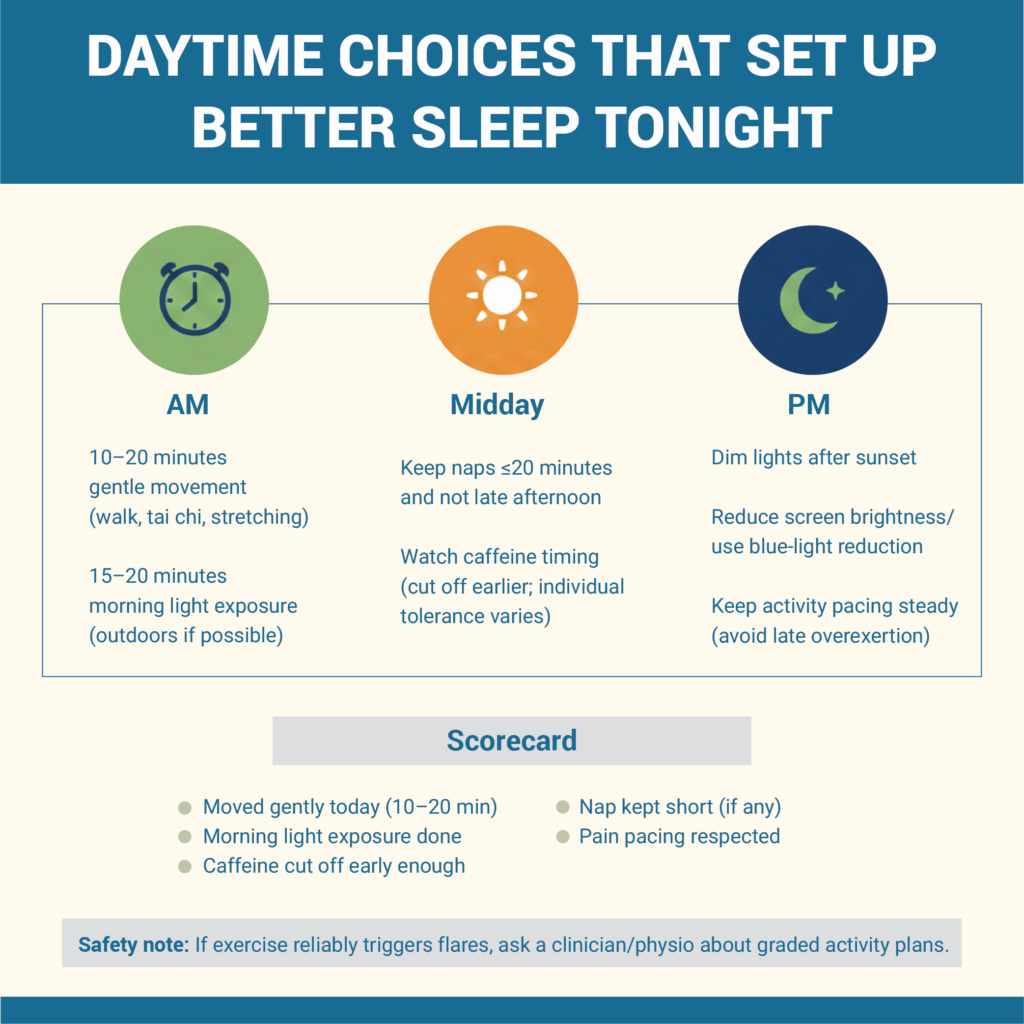
Step 7: Daytime Habits That Improve Fibromyalgia Sleep At Night (Without Triggering Flares)
Overexertion during the day can lead to increased fatigue and sleep issues at night. That is why your daytime habits must be paced to avoid triggering a flare-up. Cureus research shows that performing low-intensity exercises consistently can help fibromyalgia patients over time. However, these mobility drills must be according to your pain tolerance levels.
Follow these tips during the day:
- Gentle Movement: In the morning, include slow activities like walking, tai chi, or stretching in your routine. Do them regularly and keep the intensity low to avoid exhaustion at night.
- Sun Exposure: As soon as you wake up, get about 15 to 20 minutes of morning sun exposure. This resets your circadian rhythm and helps with cortisol management and melatonin production.
- Light Exposure: After sunset, dim the lights in your bedroom. Switch off your devices as you approach bedtime or use a blue light filter if you have to use them.
- Stimulant Awareness: Cut off your daily caffeine intake and avoid having it after noon. Also, limit alcohol, as it may impact your sleep at night.
Day-to-night Scorecard
- Did I do 10-20 minutes of exercise today?
- Did I avoid having caffeine at least 8 hours before bed?
- Did I keep my daytime nap under 20 minutes (if I took one)?
- Did I practice 5 minutes of mindfulness for sleep?
- Was my pain managed today with pacing and rest?
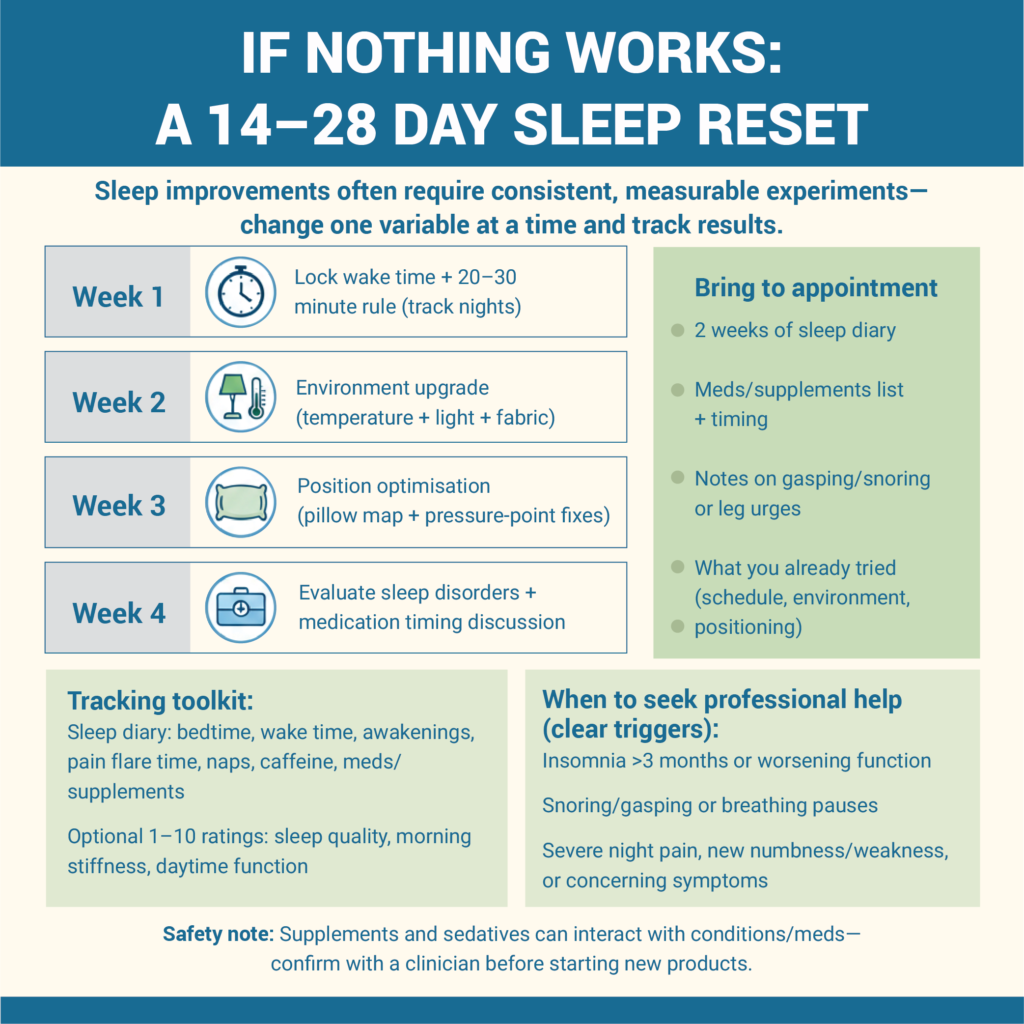
Step 8: If Nothing Works: A 2-4 Week Reset Plan, and When To Seek Professional Help
To see noticeable changes, you must follow these best practices consistently. As per a clinical study, it may take a few weeks of consistent behavioural tweaks to feel better as a fibromyalgia patient. Hence, change your routine slowly and adopt one habit at a time. This can be optimizing your pillow support or your wake-up time.
If you have tried everything and still see no improvements, you need a foolproof 2 week plan to improve sleep with fibromyalgia:
- Two-Week Test: Use a mattress topper to test out how your body reacts to new mattress firmness. You can also follow any one CBT-I technique for 14 days to see if it helps.
- Maintain a Sleep Journal: Maintain a diary to note down your bedtime, wake time, and any midnight pain flares every day.
- Annual Review: Consult a rheumatologist every year and ask them to review your prescription and symptoms.
Bring This To Your Appointment
- Sleep diary that mentions your pain patterns.
- Include the timing and dosage of all meds and supplements.
- Mention if you wake up gasping for air or have an urge to move your legs.
- Check with your doctor if your nonrestorative sleep can be linked with insomnia.
If you are constantly suffering from insomnia that has lasted for more than three months, consult a professional immediately. Many sleep-inducing supplements may impact your sleep architecture, so always consult your clinician before taking them.

Frequently Asked Questions
What is the best sleeping position for fibromyalgia pain?
Side sleeping is the most comfortable position for fibromyalgia pain, as it reduces the total body area contact with the sleeping surface. This helps reduce pressure on the spine and keeps your airways open. You can also use a pillow setup by hugging a body pillow and placing a firm pillow between your knees.
How to fall asleep with fibromyalgia insomnia if it keeps me wired?
If your brain stays alert at night despite feeling exhausted, follow a calming bedtime routine and make sure you establish a mental link with your mattress. You can practice CBT-I techniques like muscle relaxation or mindfulness to quiet a racing mind. Before bed, dim the lights and switch off your devices to reset your internal clock.
How to sleep with fibromyalgia pain at night?
If you lie awake at night due to fibromyalgia pain flare-ups, follow the “Reset-Reduce-Re-enter” model. Start by adjusting your pillow support to reduce the weight from painful areas. If you still feel uncomfortable in the next 20 minutes, get out of bed to perform a low-light activity like reading.
Do weighted blankets help with fibromyalgia sleep, and who should avoid them?
Yes, a weighted blanket can help with your fibromyalgia sleep because it applies pressure to calm the nervous system and increase serotonin. However, those with severe allodynia (where even light touch is painful), respiratory issues, or circulatory problems should avoid them.
Is melatonin or magnesium safe for fibromyalgia sleep?
Yes, melatonin and magnesium supplements are safe and effective to improve both sleep quality and pain levels in fibromyalgia patients. Magnesium helps relax muscles and supports ATP production, and melatonin helps target deep sleep. Please note that you should always consult your clinician before having them.
How long does it take to improve sleep with fibromyalgia?
Most people who make consistent changes to their sleep hygiene and routine see improvements within 2-4 weeks. With CBT-I techniques for fibromyalgia, you can see improvements in sleep quality often over a period of 8 to 12 weeks. If your sleep and pain issues persist despite making changes, schedule a medical evaluation to get targeted relief.
When should I ask for a sleep study if I have fibromyalgia?
If you notice that your sleep quality has not improved despite following good habits regularly and making support adjustments, ask for a sleep study. This will help you find fibromyalgia and restless legs syndrome, how to tell the difference, and rule out underlying health issues. A professional evaluation will guide you to manage other symptoms of sleep apnea and other disruptors more effectively with customized treatment.
Conclusion
This guide on how to sleep with fibromyalgia has shown you that you must first identify your pain patterns and causes. Check whether you suffer from chronic pain, poor sleep quality, or insomnia. Then, according to your symptoms, create a wake-up time to reset your body’s internal clock. To enhance your comfort, optimize your bedroom with the right mattress and pillow setup to protect your joints and spinal alignment. Try to sleep on your side to reduce pressure points and use breathable bedding for temperature regulation.
Keep a 2 a.m. pain plan handy to avoid waking up completely. Consult your clinician to rule out common fibro-related disruptors like sleep apnea and RLS. Follow a consistent daytime and bedtime routine, along with CBT-I, to see improvements over 2-4 weeks. If your symptoms persist, maintain a sleep journal and share it with your clinician to get the right treatment.


